From cancer data to treatment: Nancy Guo's precision medicine vision
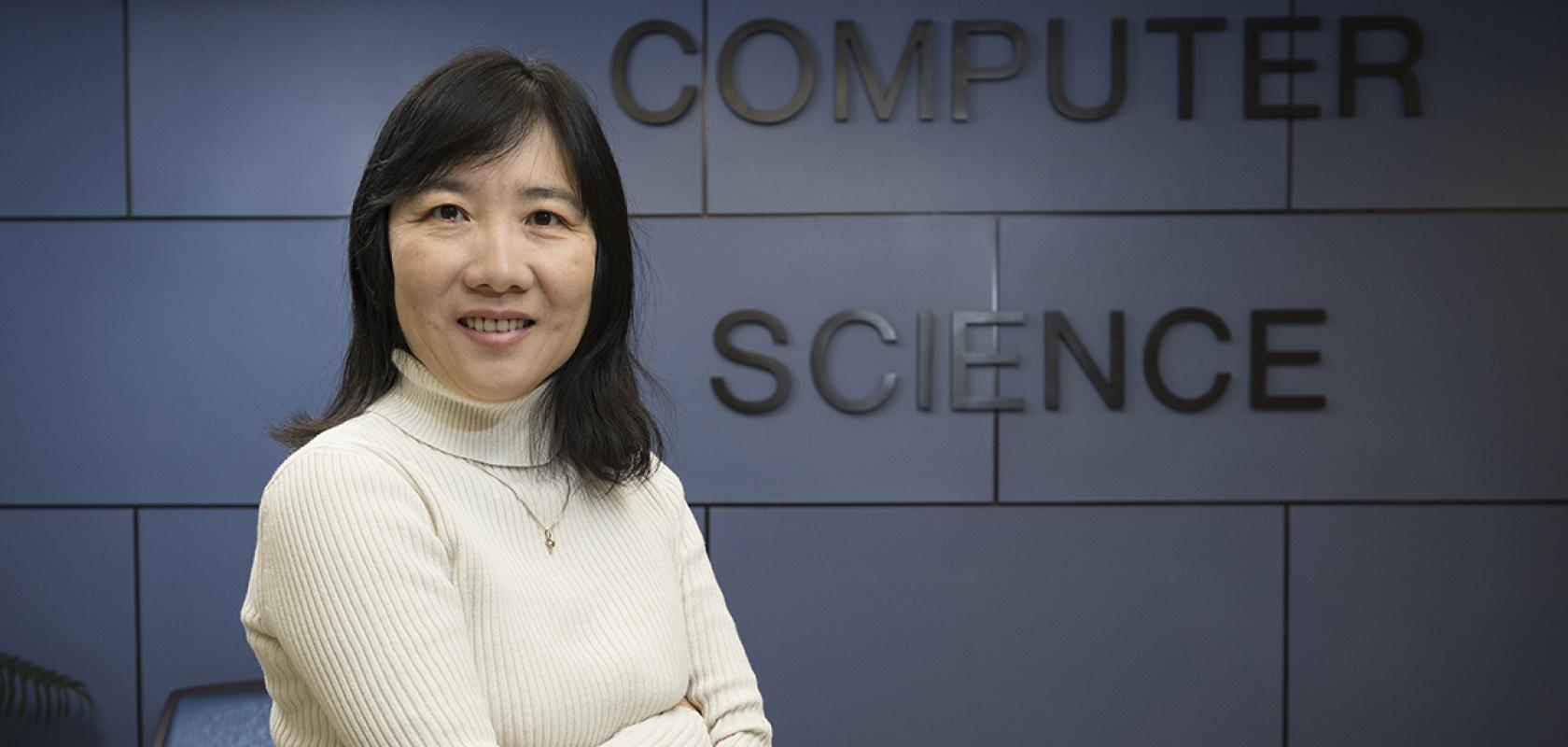
Nancy Guo, SUNY Empire Innovation Professor at the School of Computing at Binghamton University's Thomas J. Watson College of Engineering and Applied Science. (Image: Jonathan Cohen/Binghamton University)
Binghamton University’s Nancy Guo discusses the use of AI to treat cancer patients earlier, leading to better patient outcomes

Register for FREE to keep reading
Join 12,000+ scientists, engineers, and IT professionals driving innovation through informatics, HPC, and simulation with:
- Insights into HPC, AI, lab informatics & data
- Curated content for life sciences, engineering & academia
- Access to Breakthroughs: real-world computing success
- Free reports & panels, including the Lab Informatics Guide
- White Papers & software updates for smarter research
Sign up now
Already a member? Log in here
Your data is protected under our privacy policy.